APRIL 11 — A 1½-year-old girl entered the hospital’s emergency department near midnight due to salbutamol ingestion (a near bottle full). She saw the “cough” medicine served to her sister, and she stood on a chair and reached for the medication kept in a cabinet. This is the third accidental drug ingestion in the last five days. Earlier on, a 3-year-old boy with possible autism took his uncle’s pill for a chronic infection which was left on a table. Another 2-year-old boy with global developmental delay took a bottle of poorly capped eucalyptus oil. The medication splashed over the face when it tipped over. He turned cyanosed, accompanied by rapid breathing and drowsiness. The child soon developed pneumonitis (inflammation of the lung tissue because of inhalation).
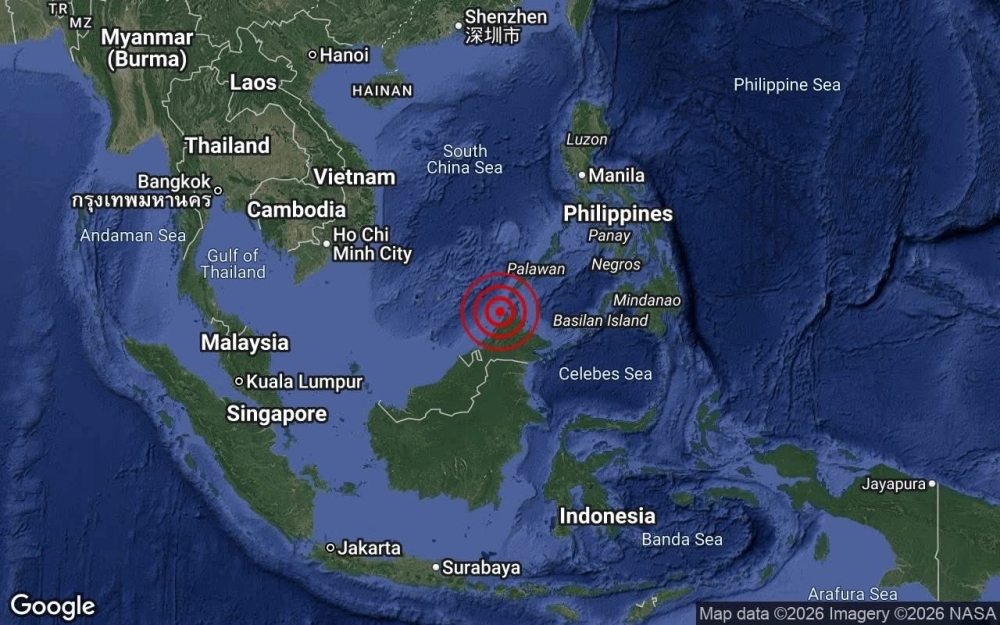
These accidents have become the by-products of the movement control order (MCO). We are unsure of how many accidents of this kind have occurred in the country, especially now we know people are avoiding an emergency department or a clinic.
But this does not come to us as a surprise. We know that home accidents (including accidental ingestion of drugs and poisons) are common among the young children. During the past month of MCO, children have been forced to stay at home with their parents who have to work from home. This may create a problem, as children who are normally cared for in a preschool, nursery or by a babysitter are potentially less supervised. The safety of this vulnerable group may have been neglected.
We are uncertain how long the MCO will go on for, but for sure, life is not the same. Children may not be able to attend a nursery or a babysitter, and parents may be asked to continue to work from home for some time. It is good to pay attention and learn strategies on childhood injuries prevention.
Preventive measures
- Do not take medicine in front of the children (because children will learn and follow), and keep all alcohol, drugs, and poisons out of sight.
- Store all medicines (and button batteries) in a locker high up (remember, children, are good at climbing to reach for things that they are curious at).
- Do not store medicines in handbags.
- Only buy medications that come with a blister pack or a safety cap. Medicines should no longer be sold in plastic bags. Do not peel off the blister pack or re-bottle them in an easy-to-open bottle or a plastic bag. These measures will minimise the harm caused in case the children do find the medicines and start to peel the tablets from the blister pack one by one and swallow them.
- Most medicines can be stored under room temperature (i.e. do not need to keep in a fridge); discard any unfinished syrup medicines (i.e. not to keep for future use).
- Do not keep cleaning agents such as detergents, dishwasher soap, antiseptics under the kitchen sink or unlocked cupboard.
- Keep cleaning agents in their original containers, with the product labels (do not re-bottle them using mineral water or Coca-Cola bottles – even adults can make mistakes and drink them accidentally).
- Store all other poisonous products such as gasoline, pesticide, or paints properly in a locked store in the garden/workplace, which are not accessible to young children.
- Allow your child to play with toys that are suitable for his age and repair any broken toys (or replace it), to prevent choking.
- Do not scatter small objects such as coins, buttons, beads – put them away from young children.
When to suspect accidental drug/poison ingestion
Drug/poison ingestion can mimic general illness in children, which includes vomiting, difficulty in breathing, or drowsiness. There may be redness around the mouth and/or lips, stains on clothing, or breaths that smell like chemicals. If the child or his siblings report the accident, do not disregard them. Be alert for clues such as empty pill bottles or packages, scattered pills, or an open toy with its battery missing.
What to do if you suspect accidental drug/poison ingestion
Get more adults to come for help.
Remember the DR ABC, where it stands for Danger removal, check for child’s Response, and assess the Airway, Breathing and Circulation.
- § Remove the child from any further dangers, such as anything remaining in the child’s mouth and contaminated clothing (do wash your hands if it is a poison).
- § Rinse the skin for 15 to 20 minutes in a shower or with a hose.
- § If the eyes are involved, gently flush the eyes with lukewarm water for 20 minutes.
Check for the child’s response. If he is well, remain calm and bring for medical attention. If the child vomits, turn his head to the side to prevent choking.
If the child is unresponsive or having the following signs, ensure someone is calling 999 for an ambulance.
- drowsy or unconscious
- difficulty in breathing or has stopped breathing
- uncontrollably restless or agitated
- seizures / fitting
Begin cardiopulmonary resuscitation (CPR) if the child shows no signs of life (e.g. moving, breathing or coughing); and to continue CPR until the ambulance or more help arrives.
During the MCO, many parents do have some free time at home. Watching and learning CPR technique from reliable online source is worthwhile.
Don’t
Do not perform any of the following practices — they are useless, and yet can cause more harm.
- induce vomit
- insert metal objects/fingers into the mouth if the child fits
- pinch the philtrum or heels attempting to wake up the child
If the child is otherwise looking well, take the child to the nearest clinic soonest possible. Do not try to perform any traditional remedy at home, which causes further delay in medical treatment.
It is vital to remain calm and do not start blaming or punishing the child (or his siblings). A scared parent and child will lead on to more harm such as accidents on the road to hospital/clinic.
Besides, do provide the doctor or ambulance officer an accurate time of ingestion of the drugs or chemicals (include button battery). Bring the original bottle, medicine package, even if they are empty. The doctor also needs to know the child’s age and weight, and the child general health condition (i.e. if he usually is taking any medicine).
While we hope the MCO will be over soon, it is good to spend the time wisely at home with the children. Do some learning together, and identify the potential dangers at home (and teach them). Parents who know their child’s character well and work with them can help to keep them safe and allow them developing to their optimal state.
Thank you.
Prof Dr Toh Teck Hock
Consultant Paediatrician & Adjunct Professor, Faculty of Medicine, SEGi University, Sibu, Sarawak
Mr Aaron Toh Aw Zien
Year 1 Medical Student, Institute of Medical & Biomedical Education, St George’s University of London
* This is the personal opinion of the writer or publication and does not necessarily represent the views of Malay Mail.