MARCH 7 ― Over the past few decades, cardiovascular disease (CVD) comprising predominantly heart attack and stroke is often perceived as a men’s disease.
Indeed, CVD influences both men and women at different magnitudes, but it is important to know that CVD is not merely a men’s disease.
For example, men typically develop CVD at a younger age as compared to women who would also acquire CVD but mostly after reaching their menopausal age.

Biologically, women of reproductive age are greatly protected against atherosclerotic CVD (ASCVD) due to the regulatory role of female hormone (oestrogen) on their cardiovascular system, directly resulting to a decreased rate of CVD events (see note 1).
However, as Malaysian women attain menopause at the average age of 50.7 years, the abrupt drop in oestrogen levels after menopause increases their risk of CVD (see note 2, 3).
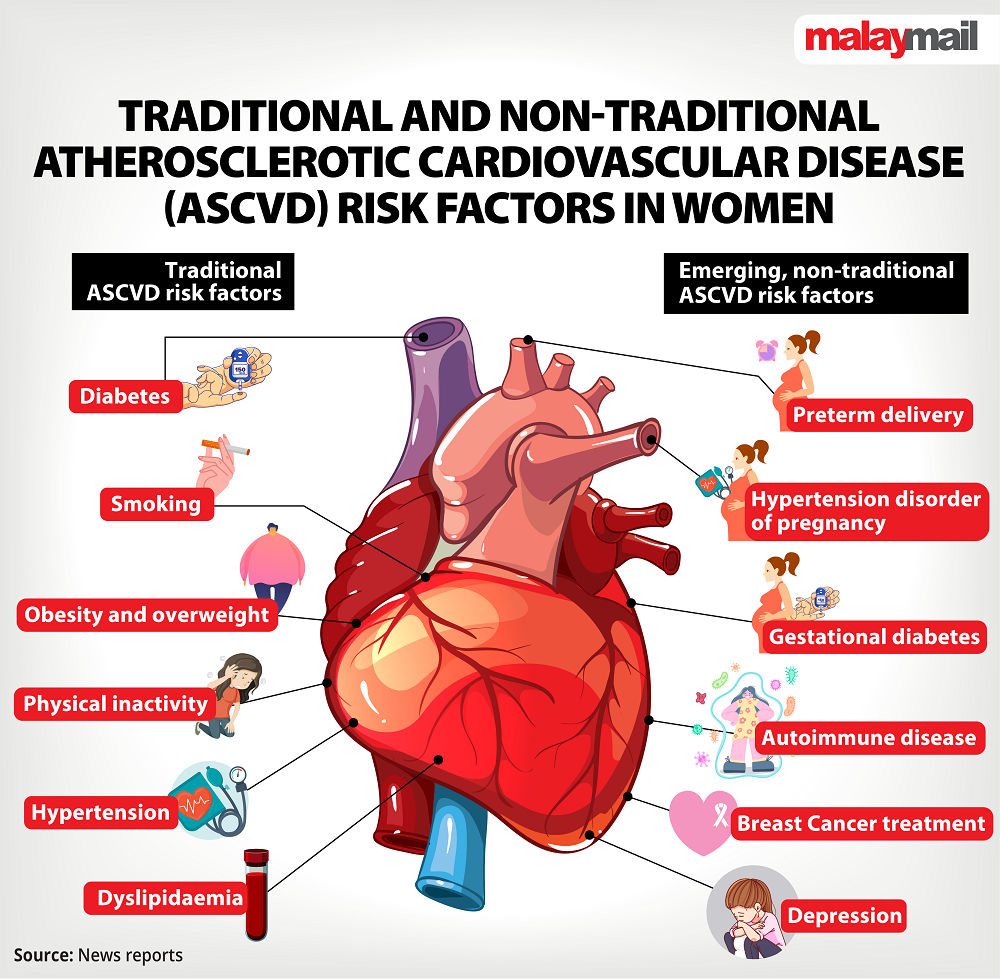
Several emerging, non-traditional ASCVD risk factors unique to women, such as premature menopause, complications of pregnancy (preterm delivery, pregnancy-induced hypertension, gestational diabetes mellitus) or breast cancer treatment may predispose these women to a higher CVD risk (Figure).
Extra attention should also be offered to young women who are disproportionately affected with autoimmune diseases (such as rheumatoid arthritis, systemic lupus erythematosus, Sjogren’s syndrome) and hence, at a higher risk of developing CVD as compared to similarly aged men.
Women have a higher tendency to self-report more CVD symptoms. Thus, establishing an initial diagnosis of CVD (particularly heart attack) is challenging among women.
This is partially attributed to the fact that majority of women reported at least three additional presenting symptoms unrelated to chest pain which may distract doctors from pinpointing the true diagnosis (see note 5)
These women were therefore less likely to receive appropriate intensification of CVD treatment, had a higher chance to be re-admitted to the hospital or even suffered from an increased chance of CVD death (see note 6).
Since the gaps in women’s cardiovascular health are multifactorial, collective commitment from the relevant stakeholders (from policymakers, non-governmental organisations, healthcare providers to public members) are required to acknowledge, educate and address the gender disparity in the healthcare setting.
In line with the upcoming International Women’s Day 2023 (observed on March 8 annually)’s campaign theme of “DigitALL: Innovation and technology for gender equality”, we should embrace the aid of technological advancements in empowering all women regarding their cardiovascular health.
Various types of mobile applications, wearable devices or social media should be promoted to women. In the long run, higher utilisation of digital health tools by women can complement the self-care concept in CVD management, thereby improving their gender-specific cardiovascular outcomes.
* The views expressed here are solely those of the writers, namely Dr Yap Jun Fai, Professor Dr Moy Foong Ming and Dr Lim Yin Cheng. They are affiliated with the Department of Social and Preventive Medicine, Faculty of Medicine, University of Malaya and the Department of Public Health, University Malaya Medical Centre.
** This is the personal opinion of the writer or publication and does not necessarily represent the views of Malay Mail.
References
1. Pérez-López FR, Larrad-Mur L, Kallen A, Chedraui P, Taylor HS. Gender differences in cardiovascular disease: hormonal and biochemical influences. Reprod Sci. 2010;17(6):511-531.
2. Clinical practice guidelines: Management of menopause in Malaysia 2022. In: Obstetrical and gynaecological society of Malaysia; 2022.
3. Peacock K, Ketvertis KM, Doerr C. Menopause (Nursing). 2021.
4. Gulati M, Hendry C, Parapid B, Mulvagh SL. Why We Need Specialised Centres for Women's Hearts: Changing the Face of Cardiovascular Care for Women. Eur Cardiol. 2021;16:e52.
5. Ferry AV, Anand A, Strachan FE, et al. Presenting Symptoms in Men and Women Diagnosed With Myocardial Infarction Using Sex-Specific Criteria. J Am Heart Assoc. 2019;8(17):e012307.
6. DeFilippis EM, Collins BL, Singh A, et al. Women who experience a myocardial infarction at a young age have worse outcomes compared with men: the Mass General Brigham YOUNG-MI registry. Eur Heart J. 2020;41(42):4127-4137.





















